Medical Practice Benchmarking, Financial Performance, and Quality Care
Medical Practice Benchmarking, Financial Performance, and Quality Care
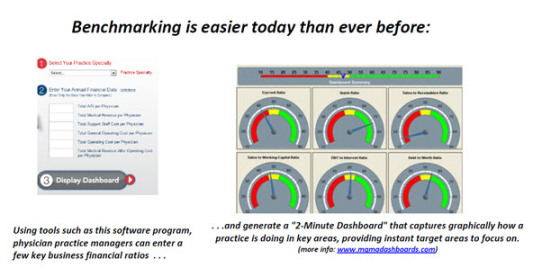
Benchmarking physician practices is an important way to assess practice value by comparing a practice’s norms to peer practices in similar specialties or in the same geographic reason. Most physician practices, according to experts, can benefit substantially from benchmarking. Moreover, it’s pretty easy to do! Here David Fein discusses what he’s discovered about the process and its benefits.
In today’s healthcare environment, cost containment is getting intense focus and attention. This is happening not only at the national level, where today’s news headlines for months have conveyed the difficulties politicians face struggling to find ways to increase healthcare coverage, while also managing costs. It’s also happening in local physician practices. With all of the changes facing the medical practice today, managing costs and increasing productivity while providing quality care has become an even more pressing issue. Physicians are faced with this dilemma: How can you provide quality care and run an efficient and profitable practice when the costs of providing medical care are going up and reimbursement levels are going down?Â
One effective and increasingly popular approach helping many physician practices better understand the financial dynamics of their practice, run those practices more efficiently, and focus more intensely on quality patient care is medical practice benchmarking.Â
Most people know that benchmarking can provide the opportunity to improve a medical group’s financial performance. However, not everyone is aware that there’s increasing evidence of a positive correlation between strong financial performance and higher quality patient care. By assessing the areas of physician compensation, production, and practice costs, and comparing a medical practice’s performance in these areas to the performance of similar practices, both regionally and nationally, physician executives and practice managers are quickly able to hone in on areas where their practice needs improvement. This insight helps practices find ways to run their offices more efficiently. The result? This can lead to smoother paths to profitability, a decrease in physician stress, and, often, a subsequent increase in the standard of patient care.Â
Efficient Management, Better CareÂ
Who can benefit from benchmarking? According to David Gans, Vice-President of Practice Management Resources at the Medical Group Management Association, 85 percent of practices can. After carefully documenting a set of best practices and surveying a broad range of the industry, MGMA found that very few of today’s practices are operating at peak performance. Benchmarking, Gans says, is “the ultimate total quality method,” because it involves not only comparing a medical group with known standards, but also mandating a continuous process of measuring and comparing performance, both internally over time and externally against other organizations and industries.Â
Good benchmarking also analyzes how best-in-class groups achieve their performance and uses that analysis as the basis to measure what a practice is doing and how it’s doing it.
Most practices find plenty of room for financial performance improvement. “Benchmarking typically identifies opportunities to save at least five to 10 percent by reducing overhead alone,” says Greg Reardon, CEO of The Reardon Group, who teaches a five-day Healthcare Consulting Workshop, that’s specifically designed to help CPAs, business valuators, and other healthcare consultants understand the unique dynamics of healthcare businesses and practice operations.Â
“When you add more efficient processes to handle physicians’ time, that in turn increases productivity, allows for additional patient visits, and can substantially increase top line revenue,” Reardon adds. Solid financial benchmarking has helped several of the practices Reardon has worked with increase their bottom lines by as much as 20 to 30 percent.Â
Also of importance is by implementing best practices and improved processes identified by these forms of analyses, practice managers can spend more time focused on issues related directly to quality of care, and physicians are able to spend more time focused on each specific patient.Â
After a practice decides to benchmark, it can choose several metrics to measure—financial performance, productivity, clinical performance, or patient satisfaction. There’s more than one way to achieve improvement within a practice. Some practices have decided to become the world’s best in a specific aspect of patient care in the belief the money will follow, even if they don’t focus on it immediately. Other practices begin by benchmarking financial performance and then turn to incorporating other forms of benchmarking.Â
This last point is particularly interesting and is an increasingly popular method. Gans, for instance, concurs with Reardon: “There is anecdotal evidence that if you do good, you can also do well.” Practices that focus on financial performance also have an unusually strong concern for maintaining excellent quality in delivering patient care.Â
Part of this may be a straightforward argument for general competence. After all, it’s logical that an effective and efficient office that runs on time and is patient-focused will provide high-quality care.Â
But whatever the reason, benchmarking is correlated not only with superior financial performance but also with quality care. Organizations that engage in benchmarking experience a collective attention shift that helps physicians and staff members focus on what is really important—optimal service to the patient. Running optimally, a practice feels less fear, engages in less frantic activity, and requires less constant management attention.Â
David Fein is CEO of ValuSource, a Colorado Springs, Colo.-based provider of business valuation and medical practice benchmarking technology.